Sepsis
Sepsis: A clinical systemic, dysregulated host response to infection. It causes extensive inflammation throughout your body that can lead to organ failure and shock if not treated with early intervention.
The term sepsis covers a broad group of conditions:
Severe Sepsis – is recognized in ICD-10 CM as Sepsis with an associated acute organ dysfunction.
Septic Shock – is recognized in ICD-10 CM as Severe Sepsis with circulatory failure associated with hypotension.
o Please refer to diagnostic criteria outlined below for specific qualifying parameters for Sepsis conditions.
SIRS – refers to the systemic response to infection, trauma/burns, or other non-infectious conditions.
Bacteremia – is the presence of bacteria in the blood.
Diagnostic Criteria
The two most recognized criteria set for Sepsis: Sepsis-2 and Sepsis-3
Sepsis-2 Criteria:
This criteria is followed by CMS and is based on the presence of infection and SIRS criteria with lab markers and findings added after the Surviving Sepsis Campaign.
Sepsis-2 criteria is when two or more of the following criteria are related to an infectious cause and cannot be explained by another co-existing condition:
- Temperature > 38 degrees C or below than 36 degrees C. (SIRS criteria)
- Heart rate >90 beats/min (SIRS criteria)
- Respiratory rate >20 breaths /min or PaCO2 < 32 mm HG (SIRS criteria)
- WBC >12,000/ul or <4000/ul or with 10% immature band forms (SIRS criteria)
- Change in mental status
- Significant edema or positive fluid balance (>20ml/kg over 24 hours)
- Hyperglycemia (>120 mg/dl) in someone without diabetes
- Elevated C-reactive protein in serum > 2 standard deviations
- Elevated procalcitonin >2 standard deviations
- Arterial hypotension (SBP <90 mmHG, MAP <70mmHg, or SBP decrease > 40mmHg in adults
Severe Sepsis markers for organ dysfunction and hypoperfusion:
- Arterial hypoxemia/PaO2/FIO2 <300
- Acute oliguria
- Creatinine Increase > 0.5 mg/dl
- Coagulation Abnormalities (INR >1.5 or PTT >60 seconds)
- Ileus
- Thrombocytopenia (Platelet count <100,000 ul)
- Lactic acid >3mmmol/L
- Hyperbilirubinemia >4
- Decreased capillary refill or mottling
Severe Sepsis with Septic Shock is recognized as hypotension, SBP <90, or MAP <70, or reduction in SBP of >40, not responsive to a fluid challenge frequently requiring vasopressor therapy. Or a lactate of >4.0.
Sepsis-3 Criteria:
The Third International Consensus Definition for Sepsis and Septic shock was released in 2016.
Per this consensus:
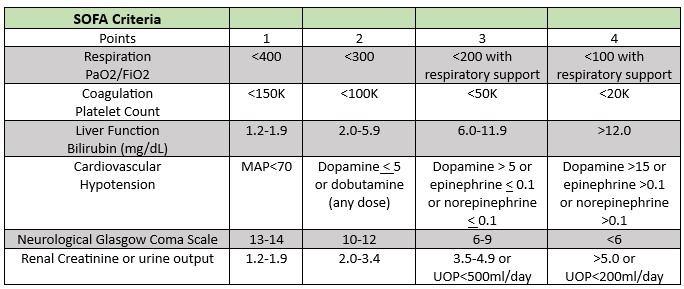
Organ Dysfunction is graded on a scaling system. The Sequential Organ Failure Score (SOFA) has a scoring system from 0-4 with 0 being no organ dysfunction beyond baseline measurement. The organ function requires a total SOFA score of 2 points or more.
The SOFA table is provided below:
Septic Shock per Sepsis 3 criteria is defined as sepsis induced hypotension despite adequate fluid resuscitation.
Septic shock requirements:
- Vasopressor support is needed to maintain a mean arterial pressure (MAP) > 65 mmHg
- Serum lactate level >2 mmol/L
Coding Considerations
Review pertinent AHA Coding Clinics for ICD-10-CM/PCS:
- Second Quarter 2020, p. 17: Sepsis due to Ventilator-Associated Pneumonia
- Second Quarter 2020, p. 28: Sepsis due to Aspiration Pneumonia
- Third Quarter 2019, p 17: Sepsis due to Multiple Possible Causes
- Fourth Quarter, 2017, p. 98: Severe Sepsis and Acute Organ Dysfunction/Failure
- Fourth Quarter 2022, p. 79: Changes to the ICD-10-CM Official Guidelines for Coding and Reporting
- Fourth Quarter 2023, p. 88: Sepsis due to Pyelonephritis of Transplanted Kidney
Review Official Coding Guidelines Chapter Specific Guidelines related to Sepsis, 1.C.1 Chapter 1:
Certain Infectious and Parasitic Diseases:
- If a patient is admitted for sepsis and a localized infection (Examples: pneumonia, cellulitis), code the sepsis first and the localized infection as secondary condition.
- R65.20 (Severe Sepsis) should only be coded if severe sepsis is documented or if organ dysfunction is linked to Sepsis.
- When a patient has severe sepsis, code the sepsis first followed by a code from R65.2 subcategory:
- 20 (Severe Sepsis without septic shock) or R65.21 (Severe Sepsis with septic shock).
A41 Other Sepsis:
Excludes 1 – Bacteriemia NOS, neonatal, puerperal sepsis, streptococcal sepsis
A41.4 Sepsis due to anaerobes:
Excludes 1 – Gas gangrene
CDI Practice Considerations
- Follow guidance from your organization on which diagnostic criteria to use for Sepsis i.e., Sepsis 2, Sepsis 3, or a combination of both. However, be aware of both sets of criteria.
- In using the SOFA scoring table, remember that 0 is based on no organ dysfunction. A patient’s baseline must be confirmed for appropriate application. For example, if a patient’s baseline creatine is 1.6 and current creatinine is 1.8, the score would be 0. If the same patient with a baseline creatinine of 1.6 has a current level of 2.5, the patient would have 1 point. The scale must be adjusted based on starting point values.
- Sepsis is a target for denials. It should always be reviewed for clinical validation. If sepsis is documented and it does not meet clinical criteria, query, as necessary.
- Negative blood cultures do not preclude a diagnosis of sepsis for patients with clinical symptoms. Refer to OCG Section 1.C.1.d.1.a.(i.)
- Organ Failure with Sepsis should be linked in documentation, query, as necessary.
- Common organ failures seen in Sepsis included, but are not limited to: Acute Renal Failure, Septic/Metabolic Encephalopathy, Acute Respiratory Failure, and Septic Shock
- If present on admission, Sepsis will most likely be the principal diagnosis. The exceptions would be if it is secondary to a complication from a device/medical care, HIV disease, newborn or pregnant patient. o Common scenarios include when patients are admitted with CAUTI’s or CLABSI, query as necessary if sepsis criteria present. In these cases, the complication code is sequenced first, with the Sepsis assigned as a Secondary diagnosis with MCC status.
- If sepsis is documented early in the record and then falls off the record, a query may be needed for consistent documentation or to indicate if sepsis has been ruled out or resolved.
- Bacteremia does not code to sepsis. Review the record closely, query, as necessary when sepsis diagnostic criteria are met.
- There is no specific code for “urosepsis” in ICD-10-CM. A query would be needed to clarify the provider’s intended diagnosis i.e., Sepsis due to UTI
- SIRS does not equate to Sepsis as there are Non-Infectious sources of SIRS. Review the record closely, if SIRS criteria are present due to an infection, either suspected or confirm, query as necessary for Sepsis (if applying Sepsis-2 criteria).
Looking for CDI help?
e4health CDI Education

Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for November’s discussion is: Strategies for Remote CDI Team Engagement. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
- Understand the challenges of remote work
- Describe the importance of engagement
- Define effective communication strategies
- Explain strategies to promote CDI team engagement
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.