Respiratory Failure
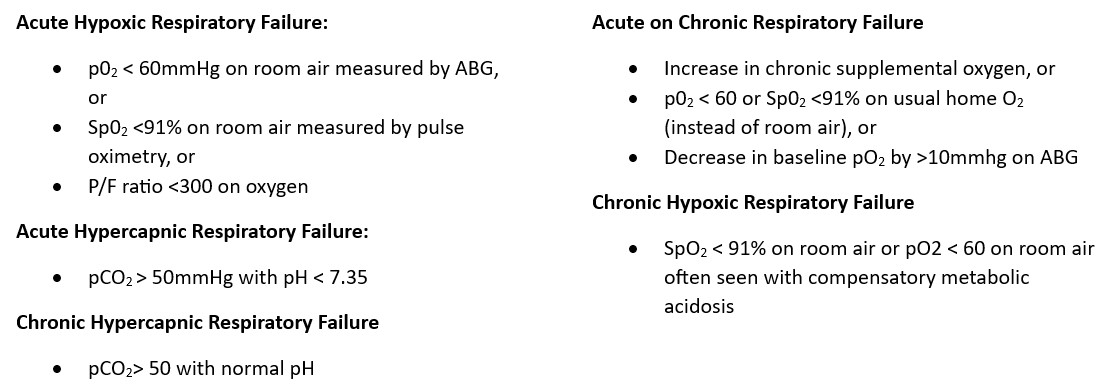
Definition: Syndrome where the respiratory systems fail in either or both the gas exchange function or oxygenation and carbon dioxide elimination. Recognized as either hypoxemic or hypercapnic.
Coding Considerations:
Review the circumstances of admission and etiology of Acute Respiratory Failure regarding assignment as principal vs secondary diagnosis. Be aware of chapter specific coding guidelines which provide sequencing guidance such as obstetrics, poisoning, HIV, and newborn.
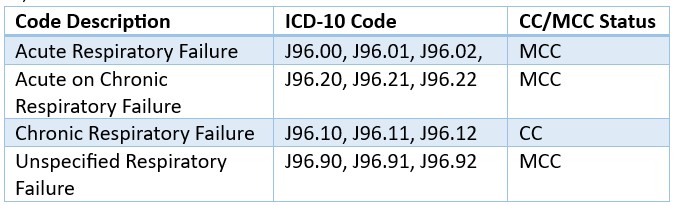
Also note: All forms of respiratory failure, even ‘unspecified,’ map to an HCC in Risk Adjustment coding
Acute Respiratory Acidosis is now indexed to Acute respiratory failure with hypercapnia (J96.02) an MCC, chronic respiratory acidosis index to chronic respiratory failure with hypercapnia (J96.12) a CC and respiratory acidosis codes to acidosis NOS (E87.29) a CC.
CDI Practice Considerations
Acute Respiratory Failure is a highly targeted diagnosis in denials. In addition to blood gas impairments, patients with acute respiratory failure should display some signs/symptoms of difficulty breathing such as: inability to speak in complete sentences, accessory muscle usage, presence of retractions, tachypnea or slowed breathing rates, breath sounds described as grunting or wheezing, or the presence of cyanosis. If unresponsive to or delayed treatment patients may also develop neurologic indications such as anxiety, confusion, restlessness, seizures, somnolence, or coma.
Mechanical Ventilation is not a requirement to diagnosis Acute Respiratory Failure, however, is a strong indicator to consider when querying along with initiation of BiPAP therapy (i.e., not used at night for routine OSA). If the patient is intubated and placed on mechanical ventilation, track the time closely ensuring documentation supports precise intubation and extubation times for accurate PCS code and MS-DRG assignment.
P/F ratios are extremely helpful for CDS’s to determine if the patient meets criteria for Acute Respiratory Failure while receiving oxygen supplementation. Further it can be a powerful tool when providing education to providers when SpO2 levels may be ‘normal’ with supplemental oxygen. It is a simple calculation:
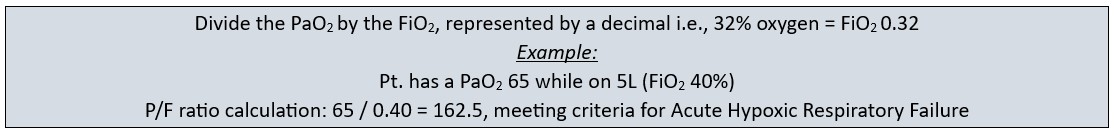
*It is inappropriate to calculate P/F ratio’s if the patient is on home oxygen therapy.
Generally accepted prediction models indicate that for every liter of oxygen supplied, the FiO2 increases by 4%.
1L = 24%
2L = 28%
3L = 32%
4L = 36%
5L = 40%
6L = 44%
Review the oxygen delivery type (NC, NRB, HFNC etc.) with flow rates closely to determine FiO2. Generally, a FiO2 of 36% or higher could be a clinical indicator for acute respiratory failure.
Acute respiratory insufficiency, acute pulmonary insufficiency, acute respiratory distress, and hypoxia do not code to acute respiratory failure. Review the record for clinical indicator support and query, as necessary.
Review clinical indicators for diagnostic criteria for Acute Respiratory Failure or Chronic Respiratory Failure when “respiratory acidosis” is documented, querying as necessary.
SpO2 ≤ 88% is a generally accepted criteria to qualify for home oxygen use, therefore when a patient requires continuous oxygen support, it is a reliable clinical indicator for chronic hypoxemic respiratory failure.
Not every patient who has COPD has chronic respiratory failure. Therefore, it is still appropriate to apply diagnostic criteria for Acute hypoxic and/or hypercapnic respiratory failure when reviewing for potential query opportunities.
Looking for CDI help?
Learn more about e4health CDI Solutions. Our Team is leading the way in the CDI industry.
e4health CDI Education
Need help to earn CEUs or education your team? Visit the IQ Education Center and get your free account or contact us for more information.
e4health is dedicated to elevating the business of healthcare. We are committed to offering support and the most current information and updates to collaborate with coding and CDI professionals to realize their fullest potential. We enthusiastically seek opportunities to develop ourselves and each other. We understand that knowledge is the key to success for our clients navigating the ever-changing health information management landscape.

Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for January’s discussion is: CDI’s Impact on Risk Adjustment and Publicly Reported Data. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
- Define CDI’s impact on risk adjustment and publicly reported data.
- Describe risk adjustment methodology.
- Identify four main websites for publicly reported data.
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.
The information and opinions presented here are based on the experience, training, and interpretation of e4health. Although the information has been researched and reviewed for accuracy, e4health does not accept any responsibility or liability regarding errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal/consulting opinion or advice.