Pneumonia
Pneumonia: An inflammation of the air sacs in one or both lungs caused by infection due to several organisms including bacteria, viruses, and fungi. It can also be caused by inhaling gases, toxic fumes, and pollutants or by aspiration. Obstructions of the bronchial tubes can cause pneumonia (tumors, small objects, food).
In the inpatient setting, the most common types of Pneumonia include:
1) Community-Acquired Pnemonia (CAP):
Acquired outside of healthcare setting, can be grouped into three categories:
- Typical bacteria:
Streptococcus Pneumoniae, Haemophilus influenzae, Staphylococcus Aures, Group A streptococci, etc.
- Atypical bacteria:
Legionella, mycoplasmapneumoniae, chlamydia pneumoniae,etc.
- Respiratory viruses:
Influenza A and B viruses, severe acute respiratory syndrome coronavirus, etc.
2) Nosocomial Pneumonia:
Acquired in a hospital setting, includes Hospital-Acquired Pneumonia (HAP) & Ventilator-Associated pneumonia (VAP):
- HAP:
Pneumonia that occurs > 48 hours after hospital admission; common causative organisms include MRSA, Pseudomonas along with other similar drug-resistant gram-negative bacteria.
- VAP:
Pneumonia that occurs > 48 hours after endotracheal intubation; common causative organisms include MRSA, Pseudomonas along with other gram-negative organisms.
3) Healthcare-Associated Pneumonia (HCAP):
- Pneumonia that was acquired in health care facilities or after recent hospitalization.
- Often documented but is no longer a recognized definition to identify treatment guidelines.
4) Aspiration Pneumonia:
- An infection of the lungs caused by the inhalation of non-air substances (food, liquid, saliva, stomach contents, etc.) into your respiratory tract.
Diagnostic Criteria
- Pneumonia is recognized as a clinical diagnosis, based on physical exam findings and symptoms.
- Imaging– CXR/CT scan typically demonstrates an infiltrate, consolidation, or interstitial changes.
- Sputum and Blood Cultures are often drawn but a conclusive organism is not typically identified from these cultures.
- Severe cases may utilize bronchoscopy and /or lung biopsy to determine cause and extent of disease.
Pulmonary Signs and Symptoms:
- Cough
- Dyspnea
- Increased Work of Breathing
- Hypoxemia
- Breath sounds (may include rales, crackles, rales)
Other Symptoms:
- Fever
- Elevated WBC
- Pleuritic chest pain
- Organ failure (in severe cases)
Coding Considerations
Review pertinent AHA Coding Clinics for ICD-10-CM/PCS:
- 1st Quarter 2017, p. 24 : Aspiration Pneumonia and Chronic Obstructive Pulmonary Disease
- 3rd Quarter, 2016, p. 15: Acute exacerbation of Chronic Obstructive Pulmonary Disease with Pneumonia
- 2nd Quarter 2020, p. 17: Sepsis due to Ventilator-Associated Pneumonia
- 1st Quarter 2017, page 25: Ventilator Associated Pneumonia and Chronic Obstructive Pulmonary Disease
- 1st Quarter, 2021, p. 25: Official Guidelines for Coding and Reporting for COVID-19
- 2nd Quarter, 2019, p. 6: Aspiration Pneumonia and Lung Transplant
- 4th Quarter, 2017, p. 96: Bacterial pneumonia, Influenza A, & Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- 2nd Quarter, 2020, p. 28 : Sepsis due to Aspiration Pneumonia
- 1st Quarter 2019, p. 8 : Human Immunodeficiency Virus and Related Conditions
Review coding considerations:
- J44.0 COPD with acute lower respiratory infection comes with instruction “code also” to identify the infection. The sequencing depends on the circumstances of the encounter.
- Lobar pneumonia should be coded to responsible organism if known. If unable to identify the organism, assign code J18.1, Lobar pneumonia, unspecified organism based on provider documentation of condition. When causal organism is not specified, lobar pneumonia can impact HCC/quality metric.
- VAP (J95.851) can only be assigned if the provider documents a link of the pneumonia to the ventilator. An additional code for the organism should be assigned.
- Pneumonia secondary to COVID -19, assign codes U07.1, COVID-19 and J12.82, Pneumonia due to COVID-19.
- If a patient is admitted with Pneumonia and has a HIV history, code the pneumonia as principal diagnosis and Z21 asymptomatic HIV status. If the pneumonia is linked to HIV as an HIV related illness, then the B20 code, HIV, would be sequenced as principal diagnosis followed by the pneumonia.
- Per ICD-10-CM Official Guidelines for Coding and Reporting, “If the diagnosis documented at the time of discharge is qualified as probable, suspected, likely, questionable, possible or still to be ruled out or other similar terms indicating uncertainty, code the condition as if it existed or was established.”
CDI Practice Considerations
- When assigned as the PDx, Pneumonia is recognized in MS-DRGs as either Simple (DRG 193-195) or Complex (177-179) which is a higher weighted DRG. Review the record closely to identify the type or causative organism, querying as necessary, as this determines code and MS-DRG assignment as well as SOI/ROM and HCC score.
- When assigned as an SDx, Pneumonia is recognized as a MCC, except for VAP, which is recognized as a CC.
Common Pneumonia Types and DRG Assignments:
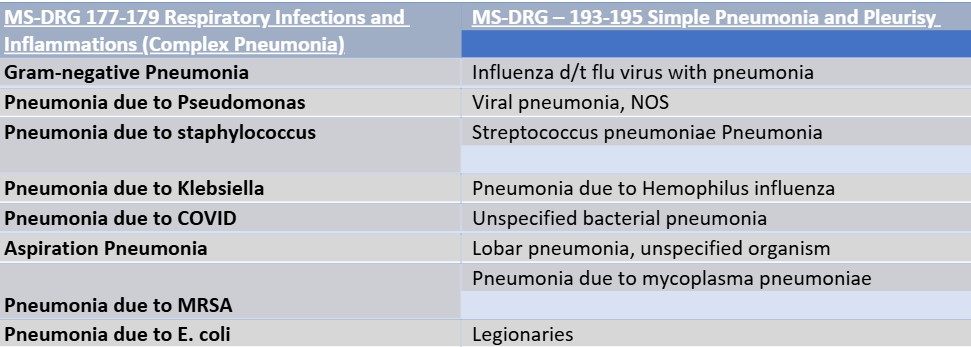
- All ‘unspecified’ pneumonias are classified as Simple Pneumonia (MS-DRG 193-195)
- Documentation of HCAP, HAP or CAP does not impact ICD-10-CM code assignment. Educate providers to document the causative organism, known or suspected.
- Certain bacterial pneumonias will map to an HCC in Risk Adjustment
- Often, providers will document HCAP or HAP thinking they are ‘saying’ the pneumonia is a gram-negative or complex pneumonia. Query as necessary when clinical indicators support a more specific pneumonia code assignment.
- Given pneumonia is recognized as a clinical diagnosis, imaging may be negative, however the provider will diagnose pneumonia based on other diagnostics. Ensure the documentation supports the providers ‘reasoning’ when clinical grounds alone are used to diagnosis pneumonia, querying, as necessary; Be aware, if a patient is dehydrated, an infiltrate and/or consolidation may not show up on imaging until the patient is adequately hydrated.
- Providers can document a cause-and-effect relationship between an organism identified in a sputum culture to pneumonia to support code assignment. However, sputum cultures can be inconclusive and are not necessary to support code assignment. The type of pneumonia can be diagnosed empirically by a provider based on patient assessment, risk factors, clinical criteria, and treatment. Also, a bacterial pneumonia cannot be coded simply based on a sputum culture or gram stain results alone.
- Review the patient’s history, clinical presentation, type of antibiotics, and response to treatment to help differentiate between a Simple or Complex pneumonia.
Common antibiotics that are used to treat pneumonia include, but are not limited to:
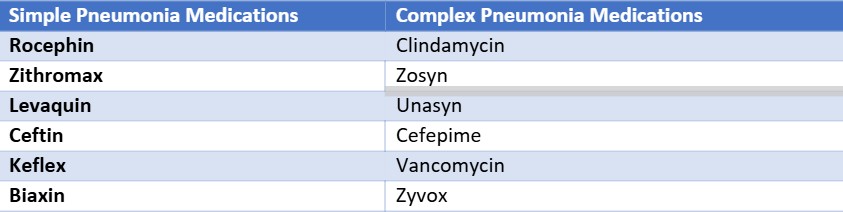
Query as necessary when clinical indicators support a more specific type of pneumonia.
Aspiration pneumonia indicators include, but are not limited to:
- Risk factors-CVA history, swallowing difficulties, coughing/vomiting, AMS
- Aspiration precautions
- Failed Speech/Swallowing Study
- Right middle and lower lung infiltrate
Other CDI Tips and Friendly Reminders:
- “Aspiration” documented alone is a symptom, not a diagnosis. Query as necessary to establish a cause-and-effect relationship to link the aspiration and pneumonia.
- Per CDC definition, Ventilator Associated Pneumonia cannot develop before 4 days of mechanical ventilation. There is not an assumed relationship between a ventilator and pneumonia. The physician must specifically document a cause-and-effect relationship, or a query will be needed.
- Both the Hospital Readmissions Reduction Program and Hospital Value -Based Purchasing 30-day mortality measures apply for a principal diagnosis of Pneumonia and Aspiration Pneumonia or a principal diagnosis of sepsis with a secondary diagnosis of pneumonia. For this Medicare population, it is important to capture secondary diagnoses for risk adjustment measures.
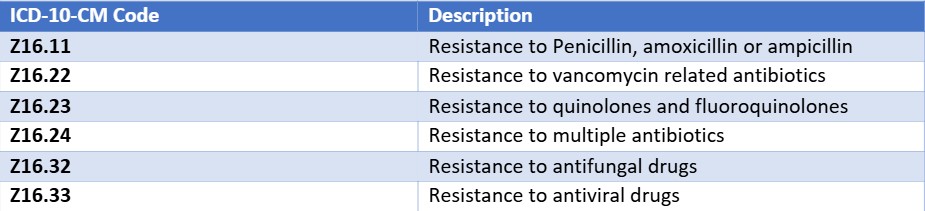
- Review for antibiotic resistance, querying, as necessary. The following ICD-10-CM codes identify resistant bacteria that are also classified as CCs. It is typical in these circumstances that more resources are used to treat the patients and the patient’s antibiotics are likely changed during the stay.
Looking for CDI help?
e4health CDI Education
Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for February’s discussion is CDI Compliance 360: Auditing for CDI Quality and Accuracy. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
- Explain the process for conducting a comprehensive Query Compliance review
- Understand the importance of missed Query Opportunities
- Describe the value of CDI Audit Reporting
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.