Myocardial Injury and Acute Myocardial Infarctions
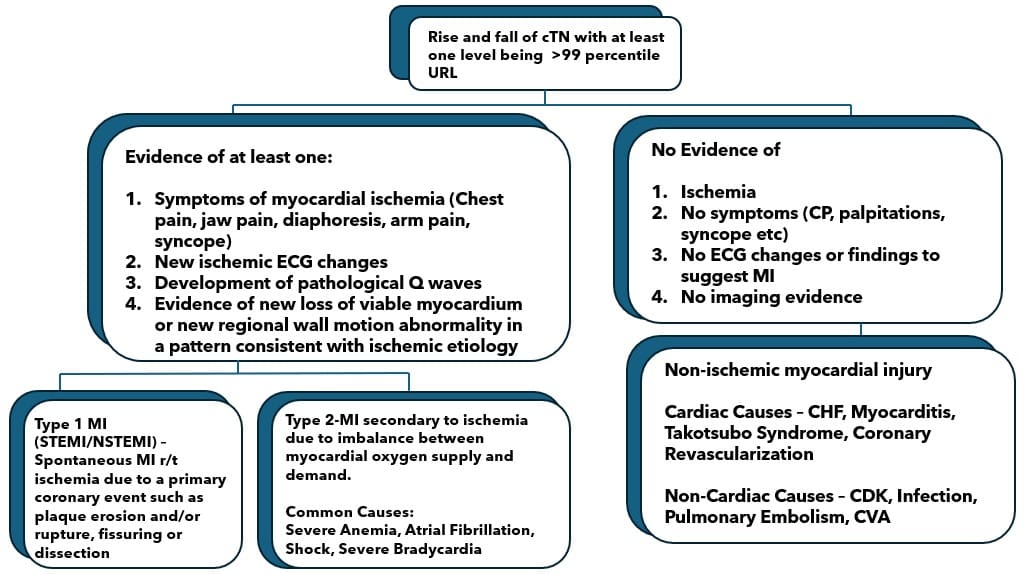
Acute Myocardial Injury: Elevated cTN value above the 99th Percentile upper reference limit (URL). The injury is considered acute if there is a rise and /or fall of cTN values.
Acute Non-Ischemic Myocardial Injury: Elevation of troponin due to non-ischemic cause, no evidence of ischemia (symptoms, ECG findings, imaging evidence).
Non-Cardiac Cause examples:
- CKD
- Infections
- Pulmonary Embolism
- CVA
- Pulmonary HTN
Myocardial Infarction: Irreversible ischemic “injury” to the myocardium that occurs when acute myocardial ischemia causes acute myocardial injury.
- Type 1 MI: Spontaneous MI related to ischemia due to a primary coronary event such as plaque erosion and /or rupture, fissuring or dissection.
- Type 2 MI: Secondary to imbalance between myocardial oxygen supply and demand. Some example causes are: Severe anemia, Shock, Hypotension, Severe Bradycardia, and Atrial fibrillation.
- Type 3 MI: Presents with MI symptoms but a troponin blood test was not performed. This type is often described as sudden cardiac death.
- Type 4a MI: Associated with percutaneous coronary intervention.
- Type 4b MI: Associated with stent thrombosis.
- Type 4c MI: Associated with restenosis (>50%) after a successful PCI.
- Type 5 MI: Associated with a CABG procedure.
- MINOCA MI: With normal coronary arteries or <50% stenosis with no obvious noncoronary cause of MI. Common causes are coronary microvascular dysfunction, spontaneous coronary dissection, plaque disruption, coronary vasospasm.
Diagnostic Criteria
Non- ischemic Acute Myocardial Injury: Rise and fall of troponin with one value of cTN above the 99% percentile.
Type 1 MI: Rise and fall of troponin with one value of cTN above the 99% percentile URL with one of following:
- Symptoms of acute myocardial ischemia: chest pain, shortness of breath, syncope, back/arm/jaw pain, diaphoresis, palpitations, profound weakness/fatigue.
- New ECG change: ST elevation, inverted T waves, etc.
- Development of pathological Q waves.
- Imaging evidence of loss of viable myocardium or new regional wall abnormalities, i.e. ECHO, MRI, CT coronary angiography, Cardiac Catheterization with angiography.
Type 2 MI: Rise and fall of troponin with one value of cTN above the 99% percentile URL and evidence of an imbalance between myocardial oxygen supply and demand unrelated to coronary thrombosis, requiring the one of the following:
- Symptoms of acute myocardial ischemia: chest pain, shortness of breath, syncope, back/arm/jaw pain, diaphoresis, palpitations, profound weakness/fatigue.
- New ECG changes: ST elevation, inverted T waves, etc.
- Development of pathological Q waves.
- Imaging evidence of loss of viable myocardium or new regional wall abnormalities.
MINOCA: Rise and fall of troponin with one value of cTN above the 99% percentile URL.
Symptoms of acute myocardial ischemia: chest pain, shortness of breath, syncope, back/arm/jaw pain, diaphoresis, palpitations, profound weakness/fatigue.
New ECG changes: ST elevation, inverted T waves, etc.
Development of pathological Q waves.
Imaging evidence of loss of viable myocardium or new regional wall abnormalities.
Non-obstructive coronary arteries (<50% stenosis).
No overt specific cause for acute presentation.
Coding Considerations
When coding I21 AMI Include codes for:
- History of Tobacco dependence or current tobacco dependence.
- Z92.82: TPA administered at a different facility.
- Excludes 2 note conditions to code: 25.2-old MI, I24.10-post-myocardial infarction syndrome, I22- Subsequent Type 1 MI.
- Type 1 MI codes are specific to site (anterior wall, inferior wall, etc.)
- Acute MI codes (I21 code grouping): Should be reported while the MI is equal to or less than 4 weeks old.
- If a type 1 NSTEMI evolves to STEM assign the STEMI code, not the NSTEMI code; If a type 1 STEMI converts to a NSTEMI due to thrombolytic therapy, it is still coded to a STEMI rather than NSTEMI code.
- A patient with Type 2 MI is assigned code I21.A1: The underlying cause of the Type 2 MI should be coded first, followed by I21.A1.
- If a Type 2 MI is described as NSTEMI or STEMI only code I21.A1.
- Type 2 MI secondary to demand ischemia or secondary to ischemic imbalance is assigned I21.A1: Do not code an additional code of I24.89 for the demand ischemia.
- If a patient has a MI secondary to in–stent restenosis: Assign T82.855A, Stenosis of coronary artery stent, initial encounter, I21.49, other myocardial type to capture the relationship of the stenosis to the culprit lesion.
- ICD-10-CM classified stenosis or narrowing of a vessel involving a previously placed stent described as “within the stent” or “in-stent” restenosis as a complication unless specifically documented as due to disease progression.
- I21.B was introduced as a new code for MINOCA in 2023.
Review pertinent Coding Clinics:
- AHA Coding Clinic ICD-10-CM/PCS Second Quarter 2023, p. 29: Myocardial Infarction and Non-Obstructive Coronary Artery.
- AHA Coding Clinic ICD-10-CM/PCS Third Quarter 2021, p. 6: Non-ST Elevated Myocardial Infarction due to Coronary Artery Disease and In-Stent Restenosis.
- AHA Coding Clinic ICD-10-CM/PCS Third Quarter 2021, p. 6: Non-ST Elevated Myocardial Infarction and In-Stent Restenosis (Culprit Lesion).
- AHA Coding Clinic ICD-10-CM/PCS Fourth Quarter 2016, p. 140: Readmission Post Myocardial Infarction.
- AHA Coding Clinic ICD-10–CM/PCS Fourth Quarter 2023, p. 25:New/Revised ICD-10-CM Codes: Coronary Microvascular Dysfunction.
- AHA Coding Clinic ICD-10-CM/PCS Fourth Quarter, 2021, p. 14: ICD-10-CM New /Revised Codes: Non-Ischemic Myocardial Injury.
CDI Practice Considerations
- Whenever a Myocardial Injury diagnosis is documented, review clinical indicator closely, ensuring adequate support is present, and query as necessary.
- Review for common comorbidities, which may include but are not limited to: Acute CHF (ensure type is specified), Cardiogenic Shock, Arrhythmias & Heart Block, Acute Respiratory Failure, and AKI.
- Acute MI (STEMI, NSTEMI, Type 2 MI, MINOCA) are MCC’s when the PDX is not another circulatory condition: Non ischemic myocardial injury is a cc (comorbid condition).
- If there is conflicting documentation between the providers, a query will need to be asked of the attending provider to clarify the diagnosis.
- Providers should be educated to document the etiology of Type 2 MI and Non-Ischemic Myocardial Injury.
- If a patient has a history of recent MI, a query may be needed to clarify the date to code the Type 1 MI that happened within the last 4 weeks.
- Acute MIs typically are MCC’s and can change the DRG: Exceptions to this rule are if it is a secondary diagnosis to a circulatory principal diagnosis.
- AMI is the driver of the MS-DRG in the circulatory system chapter: If a patient has a principal diagnosis found in the Circulatory Chapter (Heart Failure, Atrial fibrillation, DVT), The MS-DRG will be one of the MI DRGs (280-282 if discharged alive or DRG 283-285 if expired). The logic in the DRG expert book indicates DRG 280-286 is based on the principal or secondary diagnosis of I21*- Acute myocardial infarction or I22*–Subsequent STEMI & NSTEMI. For Example: If a patient is admitted with Atrial fibrillation as a principal diagnosis and had Acute MI three days into admission, the Atrial fibrillation would remain the principal diagnosis. However, the secondary diagnosis of an Acute MI would drive it to MS-DRG 282 Acute MI discharge alive without cc. The Acute MI drives the DRG but does not count as a Major comorbid condition (MCC).
- AMAMI with cardiac catheterization without any intervention will remain in MS-DRG 280-286:Any other principal diagnosis in MDC 5 circulatory system with cardiac catheterization without intervention will map to MS DRG 286-287. For Example: Acute MI with a cardiac catheterization, discharged alive-> MS-DRG 280- 282 depending on secondary diagnoses; Atrial fibrillation with a cardiac catheterization, -> MS-DRG-> 286-287 depending on secondary diagnoses.
- Keep in mind that there are MCC exclusions for DRG 283-285, Acute MI expired. These include: Cardiac Arrest due to Underlying condition, Cardiac Arrest due to other underlying condition, Cardiac Arrest, cause unspecified, Ventricular fibrillation, Respiratory arrest, Cardiogenic Shock, Hypovolemic Shock, Other Shock.
- MS-DRGs 280-282 are included in CMS quality measures related to the Hospital Readmission Reduction Program and the Hospital Value Based Purchasing Program with 30-day mortality measures.
Looking for CDI help?
e4health CDI Education
Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for February’s discussion is CDI Compliance 360: Auditing for CDI Quality and Accuracy. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
- Explain the process for conducting a comprehensive Query Compliance review
- Understand the importance of missed Query Opportunities
- Describe the value of CDI Audit Reporting
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.