Malnutrition
The term malnutrition covers 2 broad groups of conditions:
1) ‘Undernutrition’—which includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies or insufficiencies (a lack of important vitamins and minerals).
2) Overweight, obesity and diet-related noncommunicable diseases (such as heart disease, stroke, diabetes, and cancer).
Symptoms often involve weight loss, reduced appetite, tiredness, and irritability. Untreated malnutrition can cause physical or mental disability.
The 3 etiology-based nutrition diagnoses in adults in clinical practice settings are:
1) Starvation-related malnutrition: chronic starvation without inflammation (e.g., anorexia nervosa)
2) Chronic disease-related malnutrition: inflammation is chronic and of mild to moderate degree (e.g., malignancies, COPD, CKD, pancreatic insufficiency)
3) Acute disease or injury-related malnutrition: inflammation is acute and of severe degree (e.g., major infection, burns, trauma or closed head injury)
Cachexia is a hypercatabolic state defined as accelerated loss of skeletal muscle in the context of a chronic inflammatory process. It can occur in the setting of advanced cancer as well as in chronic infection, AIDS, heart failure, rheumatoid arthritis, and COPD. The weight loss by patients with cachexia cannot be entirely attributed to poor caloric intake. Cachexia and Malnutrition are not synonymous terms. A patient may or may not have both conditions.
Diagnostic Criteria
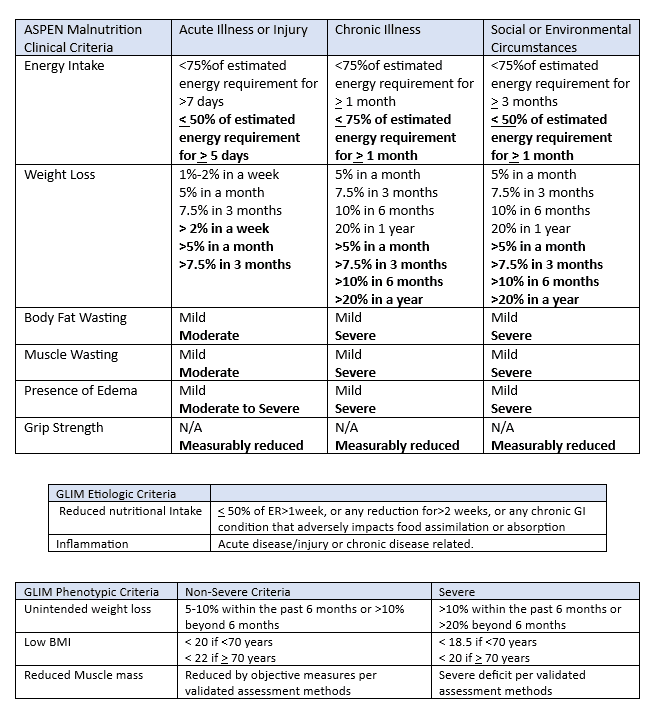
ASPEN guidelines were developed by the Academy of Nutrition and Dietetics and the American Society for Parental and Enteral Nutrition for malnutrition in 2012. The criterion for malnutrition is dependent on two criteria related to energy intake, weight loss, fat wasting, muscle wasting, edema, and grip strength (Table below) in the context of one of three scenarios; Acute illness or injury, Chronic illness or Social Circumstances as outlined in the following table with bolded criteria representing severe malnutrition and nonbolded representing non-severe (moderate) malnutrition.
GLIM (Global Leadership Initiative on Malnutrition) was developed in 2016 to build a global consensus on the core diagnostic criteria for malnutrition in adults in clinical settings. It has two etiologic criteria elements (reduced nutritional intake and inflammation) and three phenotypic criteria (% of unintended weight loss, low BMI, and reduced muscle mass). Diagnosis is based on at least one etiologic and one phenotypic criterion. Severity grading is based on the phenotypic criteria.
Coding Considerations
Review pertinent Coding Clinics such as:
- AHA Coding Clinic Fourth Quarter 2017, p. 108, Malnutrition and Malabsorption
- AHA Coding Clinic First Quarter 2020, p. 4, Malnutrition
- AHA Coding Clinic Third Quarter, 2017, p. 25, Severe Malnutrition
- AHA Coding Clinic First Quarter 2022, p. 13, Medical Treatment/Stabilization of Severe Malnutrition due to Anorexia Nervosa
- AHA Coding Clinic Fourth Quarter 2023, p. 14, New/Revised ICD-10 CM Codes: Wasting Disease (Syndrome) due to Underlying Condition.
Excludes 1 & 2 notes to be aware of for Malnutrition (E40-E46):
- Excludes 1: intestinal malabsorption (K90.-)
- Excludes 1 sequelae of protein -calorie malnutrition
- Excludes 2 nutritional anemias (D50-D53)
- Excludes 2 starvation (T73.0)
When the stage of malnutrition has progressed from mild to moderate or mild/moderate to severe, assign one code to capture the highest level of severity. THE POA indicator of “Y” would apply to highest severity.
The diagnosis of malnutrition impacts risk adjustment within the HHS-HCC methodology.
When coding malnutrition/cachexia, also code the BMI, if documented
The terms “Malnourishment” or “Malnourished” are not found in the ICD-10-CM Alphabetic Index however should be coded the same as ‘Malnutrition’. (AHA Coding Clinic First Quarter 2020, page 6)
The term “Cachectic” is not found in the ICD-10-CM Alphabetic Index however should be coded the same as ‘Cachexia’. (AHA Coding Clinic Third Quarter 2006, page 15)
CDI Practice Considerations
- Malnutrition can impact DRG assignment, as Mild, Moderate, or Unspecified malnutrition (E44 code group) provides a CC as a secondary diagnosis, while Severe Malnutrition (E43) provides a MCC as a secondary diagnosis.
- Severe malnutrition is a highly targeted diagnosis for denials. A Clinical Validation Query of malnutrition, any severity level, may be needed if there is a discrepancy between the provider and nutrition therapy regarding the diagnoses or if clinical indicators do not support current documentation, query, as necessary.
- CDI programs should work with their organization to develop a standardized definition for malnutrition at their hospital- this may be ASPEN, GLIM, or a combination of both.
- Develop a close relationship with nutrition therapy to identify patients with malnutrition so they are accurately diagnosed, treated and malnutrition diagnosis with severity is captured in documentation and code assignment. Refer to OCG Section 1.B.14, as a query may be needed to obtain diagnosis for code capture.
- Be aware of conditions that are commonly associated with malnutrition, which may include, but are not limited to: Dementia / Malignancies / Short Gut Syndrome / S/P Bariatric Surgery / Gastrointestinal symptoms (nausea, vomiting, diarrhea) / Prolonged NPO status
- Depending on criteria utilized, BMI may not be one of the criteria to rely on for diagnosis of malnutrition. Be aware, a patient can be malnourished with a high or normal BMI.
- When educating providers on documentation, encourage the documentation of treatment of malnutrition as well as supportive criteria from the nutrition consult.
- E40, E41 and E42 (kwashiorkor, nutritional marasmus and marasmic kwashiorkor) are rarely seen in the United States. Ensure documentation supports code assignment, querying when necessary.
- Cachexia and Malnutrition can be reported together and often co-exist clinically. Although Cachexia is designated as a CC when assigned as a secondary diagnosis, adding both may further impact risk adjustment methodologies impacting reputational data. Likewise, capture of underweight, R636 or abnormal weight loss, R634 do not impact DRG assignment on their own, only if paired with the Z68.1, BMI 19.9, can provide a CC when assigned as a secondary diagnosis, however on their own R636 & R634, can impact risk adjustment methodologies and reputational data.
Looking for CDI help?
e4health CDI Education

Click here to register!
Learning Objectives:
- Identify non-compliant query practices
- Explain how to transform non-compliant queries into compliant queries
- Understand when to use Yes/No query formats
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.