Encephalopathy
Encephalopathy: “Any diffuse disease of the brain that alters brain function or structure” according to the National Institute of Neurological Disorders of Stroke.
The term encephalopathy covers two broad groups of conditions:
Acute encephalopathy – is due to systemic factors that will resolve once the etiology is found and corrected.
Chronic encephalopathy – is generally a slow progression of altered mental status.
Acute encephalopathy types include the following:
- Metabolic Encephalopathy – caused by a metabolic derangement in conditions such as electrolyte imbalance, infection, hypoglycemia, organ dysfunction and failure, acute hypoxia
- Toxic Encephalopathy – due to medicine, illicit drugs, toxic chemicals
- Hepatic Encephalopathy – neurological impairment related to elevated ammonia levels in end stage liver disease
- Wernicke-Korsakoff Syndrome – due lack of thiamin (Vitamin B1) often seen with alcohol use disorders & malnutrition
Chronic encephalopathy types include the following:
- Alcoholic Encephalopathy – chronic due to long term use of alcohol
- Anoxic Encephalopathy – permanent brain damage due to prolonged hypoxia
- Chronic Traumatic Encephalopathy – post-concussion syndrome
- Hypertensive Encephalopathy – acute severe hypertensive episode causing headache and confusion, which can progress to stupor or a state of unresponsiveness. Convulsions can also be seen in some cases
Diagnostic Criteria
Acute Encephalopathy Hallmark Signs:
o Acute generalized alternation in brain function
o Deviating from baseline
o Described as altered mental status that resolves when the underlying etiology is treated
o Not due to structural brain disease or changes
Altered Mental Status can be seen or described as a combination of, but not limited to:
o Confusion, disoriented
o Lethargic, decreased alertness, not able to concentrate, obtunded
o Loss of memory and cognitive ability
o Change in behavior, speech, or personality
Coding Considerations
Excludes 1 & 2 notes to be aware of for Encephalopathy Malnutrition:
G93.4 – Other and unspecified encephalopathy – Excludes 2:
- G31.2 – alcoholic encephalopathy
- G94 – encephalopathy in diseases classified elsewhere
- I67.4 – hypertensive encephalopathy
- G92.8 – toxic (metabolic) encephalopathy
G92.8 – Other toxic encephalopathy & G92.9 Unspecified toxic encephalopathy:
- T36-T65 – code first poisoning due to drug or toxic, if applicable, with fifth or sixth character 1-4 or 6
- T36-T50 – use additional code for adverse effect, if applicable to identify drug, with fifth or sixth character 5
I67.4 – Hypertensive encephalopathy includes an Exclude 2:
- G45.2 – insufficiency, NOS, of precerebral arteries
K76.82 – Hepatic encephalopathy, Code also any underlying liver disease – Exclude 1:
- K72.01 – acute and subacute hepatic failure with coma
- K70.41 – alcoholic hepatic failure with coma
- K72.11 – chronic hepatic failure with coma
- K72.91 – hepatic failure with coma
Review pertinent Coding Clinics such as:
AHA Coding Clinic ICD-10-CM/PCS Second Quarter 2024, p. 14-15, Metabolic Encephalopathy with Metabolic Toxic Encephalopathy
AHA Coding Clinic ICD-10-CM/PCS Second Quarter 2018, p. 24, Clarification: Encephalopathy Caused by Other Conditions
AHA Coding Clinic ICD-10-CM/PCS Second Quarter 2017, p. 8, Encephalopathy due to Sepsis
AHA Coding Clinic ICD-10-CM/PCS First Quarter 2022, p. 52, Toxic Metabolic Encephalopathy due to Hepatic Encephalopathy
AHA Coding Clinic, ICD-10-CM/PCS First Quarter 2017, P. 39, Toxic Encephalopathy due to Adverse Effect of Ciprofloxacin
AHA Coding Clinic, ICD-10-CM/PCS Fourth Quarter 2018, p. 16, ICD-10-CM New/Revised Codes: Lacunar Infarction
AHA Coding Clinic, ICD-10-CM/PCS, Second Quarter 2021, p. 3, Static Encephalopathy due to epilepsy
CDI Practice Considerations
Review the record closely, identifying the TYPE or CAUSE of the encephalopathy and query, as necessary:
Be aware: if encephalopathy is due to two separate causes, metabolic encephalopathy, and toxic encephalopathy, can be coded together. However, when due to the same etiology, assign only code G92.8, other toxic encephalopathy. (see coding clinic referenced above)
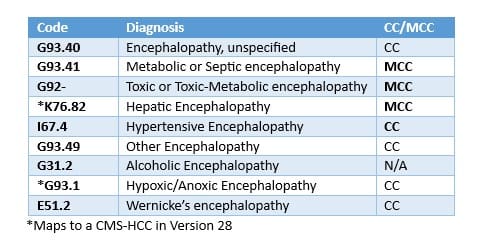
Recognized by type/etiology in ICD-10, encephalopathy codes having varying CC/MCC status when assigned as a Secondary Diagnosis, for example:
When the primary reason for the patient’s admission is due to Encephalopathy, if specified as:
o Metabolic, Other, and Unspecified Encephalopathy: Map to DRGs 070-072
o Toxic:
If due to a poisoning, overdose, or toxic effect, the poisoning code would be sequenced first mapping to DRG 917, as G92-, Toxic encephalopathy assigned as a Secondary Diagnosis (MCC). If due to an adverse effect, G92-, Toxic encephalopathy would be assigned as the Principal Diagnosis, mapping to DRGs 089-091, with the Adverse Effect (T36-T50) code assigned as a Secondary Diagnosis.
Encephalopathy, especially if specified as metabolic, toxic, toxic-metabolic, are highly targeted diagnoses seen in denials, given MCC status:
- Clinical Validation reviews are crucial, review the record closely ensuring clinical support is evident querying when necessary.
- Educate providers to document not only the type and cause of encephalopathy as well as the patient’s baseline and when they return to normal. This is especially important for dementia patients.
Dementia patients can have acute encephalopathy, when an alteration occurs where they deviate from their baseline, that is due to a metabolic, drug-related, or toxic etiology, that once corrected return to their baseline:
- Determining a patient with dementia’s normal baseline is key, review the H&P closely as baseline may be reported by family members, and nursing notes can further support if a true change has occurred, as well as when the patient has returned to their normal baseline.
- Example: Metabolic encephalopathy secondary to UTI in dementia patient, patient returning to baseline after treatment with IV antibiotics and IV fluids.
Treatment is a key factor in support of encephalopathy and will help determine the type or etiology. Given structural changes do not occur in acute encephalopathy, often time CT/MRI’s will be unremarkable. EEG may demonstrate slowing, however likely will not be ordered on every encephalopathic patient. Review diagnostic work up, to identify any medication/toxic abnormalities, electrolyte irregularities, or infectious process.
When encephalopathy is documented and linked to a condition, review for clinical support and query as appropriate to further specify the type of encephalopathy:
- Example: Encephalopathy secondary to UTI documented > G93.49, Other Encephalopathy (CC) Vs. Metabolic encephalopathy secondary to UTI > G93.41, Metabolic Encephalopathy (MCC)
Wax and waning are not characteristic of acute encephalopathy, instead more typical of sundowning.
Encephalopathy due to Sepsis represents Organ Failure. Based on clinical indicator support, query as necessary to clarify the type/etiology of Encephalopathy as Septic.
This allows code assignment of G93.41, Metabolic Encephalopathy, as well as R65.20, Severe sepsis without septic shock:
- Be aware of: Glasgow Coma Scores in patients with confusion if applying Sepsis- 3 Sofa criteria.
Looking for CDI help?
e4health CDI Education

Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for November’s discussion is: Strategies for Remote CDI Team Engagement. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
O Understand the challenges of remote work
O Describe the importance of engagement
O Define effective communication strategies
O Explain strategies to promote CDI team engagement
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.