Coma
Definition: Deep state of unconsciousness where patients are unable to move or be aware of or respond to their surroundings with loss of thinking abilities however retain non-cognitive function and normal sleep patterns.
Diagnostic Criteria
A comprehensive neurological examination is required. A Glasgow Coma Scale (GCS) score of 8 or less is generally accepted as diagnostic criteria supportive of the diagnosis of Coma.
The GCS is a widely adopted system to measure consciousness. It consists of three categories, with the highest score 15 indicating awake/alertness versus the lowest score of 3 indicating a severe coma.
- Eye response (score 1-4)
- Motor response (score 1-5)
- Verbal response (score 1-6)
Additional diagnostic testing may be conducted to determine etiology and treatment modality. These may include:
- Diagnostic imagining such as Head CT or Brain MRI-to identify structural intracranial disease.
- Laboratory testing of blood, urine, CSF fluid-to identify a metabolic derangement such as electrolyte imbalances, infections, or the presence of toxics/poisons.
- Electroencephalogram (EEG)-reviewing for seizures or epilepsy as potential cause.
Coding Considerations:
Review pertinent Coding Clinics such as:
- AHA Coding Clinic, Fourth Quarter 2021, p. 112 Unspecified Coma
- AHA Coding Clinic, Fourth Quarter 2021, p. 113 Medically Induced Coma
- AHA Coding Clinic, Second Quarter 2021, p. 4 Multiple Glasgow Coma Scale Scores Pre and Post Admission
- AHA Coding Clinic, Third Quarter 2020, p. 46 Partial Glasgow Coma Score
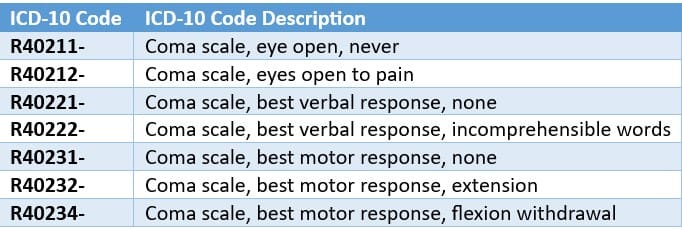
The coma scale codes (R40.21-R40.24) can be used in conjunction with traumatic brain injury codes. These codes are primarily for use by trauma registries; however, they may be used in any setting where this information is collected. The coma scale codes should be sequenced after the diagnosis code(s). These codes, one from each subcategory, are needed to complete the scale. The 7th character indicates when the scale was recorded. The 7th character should match for all three codes. Many of these R codes also map to an HCC and can affect Risk Adjustment scores.
CDI Practice Considerations
Review documentation for the etiology of the coma as well as potential complications or comorbidities.
Etiology of Coma can include, but is not limited to:
- Traumatic Head Injury
- Stroke
- Oxygen depletion to brain (severe hypothermia or drowning)
- Infections (Encephalitis, meningitis)
- Toxic Substance (carbon monoxide poisoning, drug/alcohol overdose)
- Complication of an underlying disease process such as diabetes with blood glucose level too high or low
- Repeated seizure
When reviewing coma patients, pay close attention to documentation opportunities for comorbidities associated with each body system. Some to keep in mind include:
- Respiratory: Acute Respiratory Failure; Pneumonia
- Kidney/Urinary Tract: UTI
- Endocrine: Malnutrition
- Musculoskeletal: Functional Quadriplegia
- Skin: Pressure Injuries
- Infection/Generalized: Sepsis
Terms that may be documented to describe a patient in a coma include “unresponsive,” “obtunded,” “stupor,” “somnolent”, or “locked-in syndrome”. Review the record closely for clinical indicators and treatment, querying the provider for clarification when appropriate.
When all components are known, do not assign a code for the total GCS, as it is not designated CC/MCC status. Instead Reporting individual components are classified as MCC’s, shown in the following:
GCS can be assigned based on documentation from non-providers (see ICD-10 Official Coding Guidelines 1.B.14 ‘Documentation by Clinicians Other than the Patient’s Provider’). However, the patient’s provider must document the actual diagnosis of coma and etiology. If there is conflicting medical record documentation, either from the same clinician or different clinicians, the patient’s attending provider should be queried for clarification.
Coma is classified as a MCC while persistent vegetative state is classified as a CC.
Since the term ‘unconsciousness’ is assigned to coma, unspecified (R4020), a thorough review of the record needs to be completed, clinically validating the diagnosis. If the significance of the unconsciousness is unclear, query the provider.
Code R40.20, unspecified coma, may be assigned in conjunction with codes for any medical condition, except for neonatal coma (P91.5) and coma in diabetes (E08-E13), in hepatic failure (K72.-) or nondiabetic hyperglycemia (E15).
ICD-10 classifies several conditions as combination codes that contain ‘with coma’. Review the record closely for clinical indicators and treatment querying when appropriate as the following combinations codes are designated as MCC’s:
- Hepatitis A with hepatic coma (B150)
- Acute hepatitis B with delta-agent with hepatic coma (B160)
- Acute hepatitis B without delta-agent with hepatic coma (B162)
- Acute hepatitis C with hepatic coma (B1711)
- Unspecified viral hepatitis with hepatic coma (B190)
- Unspecified viral hepatitis B with hepatic coma (B1911)
- Unspecified viral hepatitis C with hepatic coma (B1921)
- Diabetes mellitus due to underlying condition with hyperosmolarity with coma (E0801)-when POA
- Diabetes mellitus due to underlying condition with ketoacidosis with coma (E0811)-when POA
- Diabetes mellitus due to underlying condition with hypoglycemia with coma (E08641)
- Drug or chemical induced diabetes mellitus with hyperosmolarity without nonketotic hyperglycemic hyperosmolar coma (E0900)-when POA
- Drug or chemical induced diabetes mellitus with hyperosmolarity with coma (E0901)-when POA
- Drug or chemical induced diabetes mellitus with ketoacidosis with coma (E0911)-when POA
- Drug or chemical induced diabetes mellitus with hypoglycemia with coma (E09641)
- Type 1 diabetes mellitus with ketoacidosis with coma (E1011)-when POA
- Type 1 diabetes mellitus with hypoglycemia with coma (E10641)
- Type 2 diabetes mellitus with hyperosmolarity with coma (E1101)-when POA
- Type 2 diabetes mellitus with ketoacidosis with coma (E1111)-when POA
- Type 2 diabetes mellitus with hypoglycemia with coma (E11641)
- Other specified diabetes mellitus with hyperosmolarity with coma (E1301)-when POA
- Other specified diabetes mellitus with ketoacidosis with coma (E1311)-when POA
- Other specified diabetes mellitus with hypoglycemia with coma (E13641)
- Alcoholic hepatic failure with coma (K7041)
- Toxic liver disease with hepatic necrosis, with coma (K7111)
- Acute and subacute hepatic failure with coma (K7201)
- Chronic hepatic failure with coma (K7211)
- Hepatic failure, unspecified with coma (K7291)
Looking for CDI help?
Learn more about e4health CDI Solutions. Our Team is leading the way in the CDI industry.
e4health CDI Education
Need help to earn CEUs or education your team? Visit the IQ Education Center and get your free account or contact us for more information.
e4health is dedicated to elevating the business of healthcare. We are committed to offering support and the most current information and updates to collaborate with coding and CDI professionals to realize their fullest potential. We enthusiastically seek opportunities to develop ourselves and each other. We understand that knowledge is the key to success for our clients navigating the ever-changing health information management landscape.

Earn FREE ACDIS CEUs when you join Staci Josten, RN, BSN, CCDS, Alyson Swinehart, BSN, RN, CCDS, and other CDI leaders for a roundtable discussion regarding important, timely industry topics! The topic for January’s discussion is: Advancing your CDI Program with Second Level Reviews. We will provide background on this topic, share industry insights, and facilitate collaborative discussion with guided questions and answers.
Click here to register!
Learning Objectives:
- Describe an effective Second Level Review Process
- Identify the types of Second Level Reviews
- Explain the value of a robust Second Level Review
What is the e4health CDI Leadership Roundtable?
The goal for the virtual CDI Leadership Roundtable Discussion is for CDI leaders to explore specific topics within CDI, learn about the topic and from each other. During each roundtable, e4health CDI Leader’s will present a CDI topic, spend time sharing current industry standards or some education regarding this topic and then open with probing questions for group discussion.
Who should attend the e4health CDI Leadership Roundtable?
The focus of this group is for those who have influence over CDI program process, policy, and education.
Why should I attend the e4health CDI Roundtable?
This will be a wonderful place to learn, share your wins and challenges and collaborate with other CDI leaders across the industry. Also, after completing a survey, free ACDIS CEUs will be earned.
The information and opinions presented here are based on the experience, training, and interpretation of e4health. Although the information has been researched and reviewed for accuracy, e4health does not accept any responsibility or liability regarding errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal/consulting opinion or advice.