Technology & AI Enabled Services
Harness the Power of AI and Automation in Healthcare
Helping healthcare providers unlock the power of artificial intelligence (AI) in revenue cycle safely, quickly, and effectively.
Empowering Better Health Through Innovation
Addressing Healthcare Challenges with AI

Overcoming Talent Shortages
Our AI solutions mitigate the impact of medical coding talent scarcity by automating complex coding processes, ensuring accuracy and efficiency.

Reducing Administrative Costs
Streamline administrative tasks with AI-driven automation, significantly reducing overhead expenses and allowing staff to focus on patient care.

Optimizing IT Resources
Alleviate IT resource constraints and manage project overload with intelligent automation, freeing up your team to tackle strategic initiatives.
Artificial Intelligence Continuum in Healthcare
Technology
Robotic Process Automation (RPA)
Machine Learning (ML)
Natural Language Processing (NLP)
Ambient & Conversational AI
Generative AI (GenAI)
Description
Automation of repetitive, rule-based tasks using software robots
Algorithms that learn from data to make predictions or decisions
AI that understands, interprets, and generates human language
AI that integrates into the environment, listening & has contextual awareness
AI that creates new content such as text, images, or code
Application
- Data entry for billing
- Appointment scheduling
-
Predicting patient no-shows
-
Fraud detection
- Automated patient comms
- Transcribing medical records
-
Patient visit note capture & summary
-
Virtual health assistants and chat bots
-
Generating medical documents
-
Creating personalized patient education materials
Transformative AI Solutions for Healthcare
Strategic AI and Automation Solutions
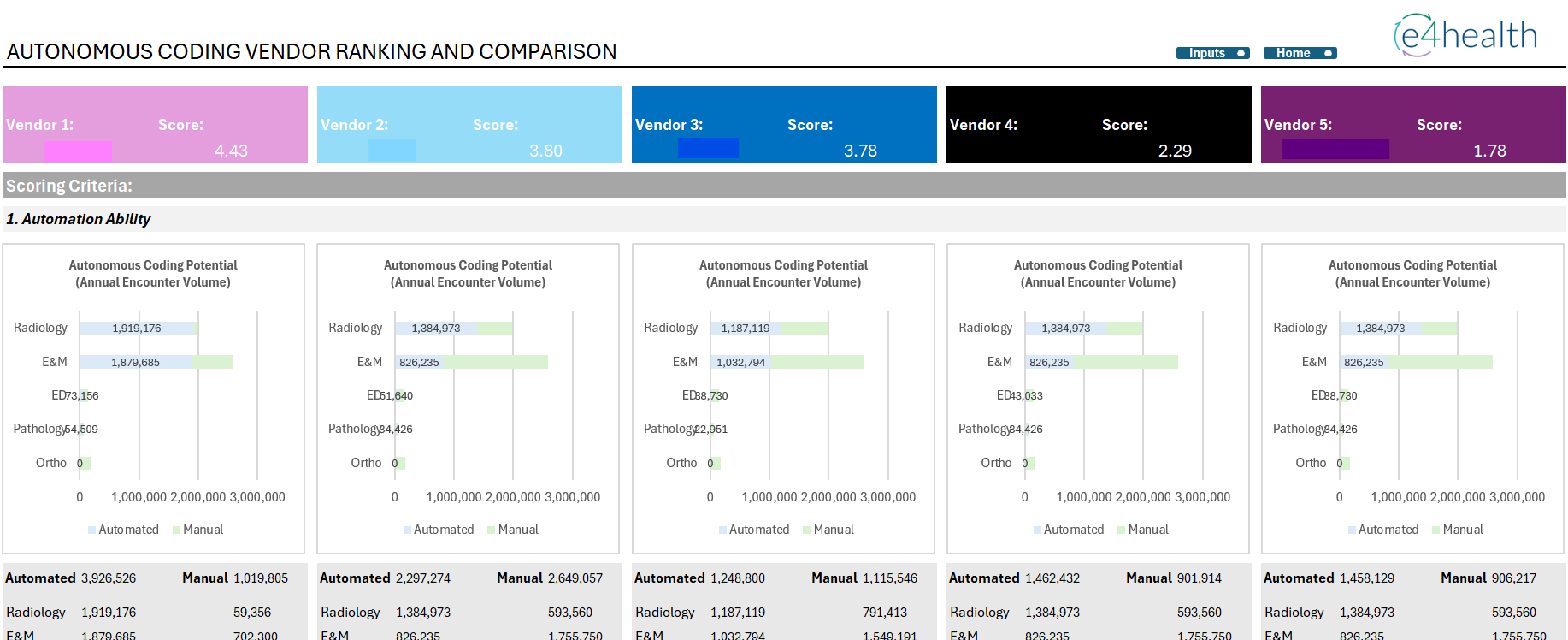
Technology & AI Enabled Medical Coding
Our AI-driven full-service coding solutions automate the mundane while delivering operational efficiency and cost savings without sacrificing quality.
Patient Access
Utilize Robotic Process Automation and Natural Language Processing to improve operational efficiency, reduce data extraction errors, and enable faster decision making.
Clinical Documentation Integrity
Enhance clinical documentation accuracy with AI-powered tools that help identify documentation deficiencies and coding errors, reducing denied claims and enabling accurate financial outcomes.
AI Assessment
Leverage e4health’s third party subject matter expertise to identify areas where AI can drive operational efficiency gains and improvements.
Unlock AI Potential with Our Expert Assessment
Discover how e4health can transform your healthcare operations with cutting-edge AI solutions. Request an AI assessment today to explore tailored strategies that enhance efficiency, accuracy, and patient care. Empower your organization with our expertise and drive meaningful change.

Prepare for the Future of Healthcare
Explore how e4health is helping our customers prepare for the future of healthcare with AI and automation. Dive into our journey and see how technology is shaping better health outcomes.